
Emergency Dentist Basingstoke
Dental problems don’t always wait for a convenient time. Whether it’s sudden tooth pain, a broken filling, or an accident that’s damaged your smile, you need care you can count on—quickly and calmly. That’s exactly what we offer at Hampshire Dental Care.
If you’re looking for a reliable emergency dentist in Basingstoke, our experienced team is here to help you with same-day appointments, honest advice, and expert treatment. We also regularly support patients from Farnham and the surrounding areas who need urgent dental care and don’t want to wait for a hospital visit or NHS referral.
We understand that dental emergencies can be stressful, so we prioritise fast access, gentle care, and a clear plan to get you out of pain and back to normal.
Do I Need Emergency Dental Treatment?
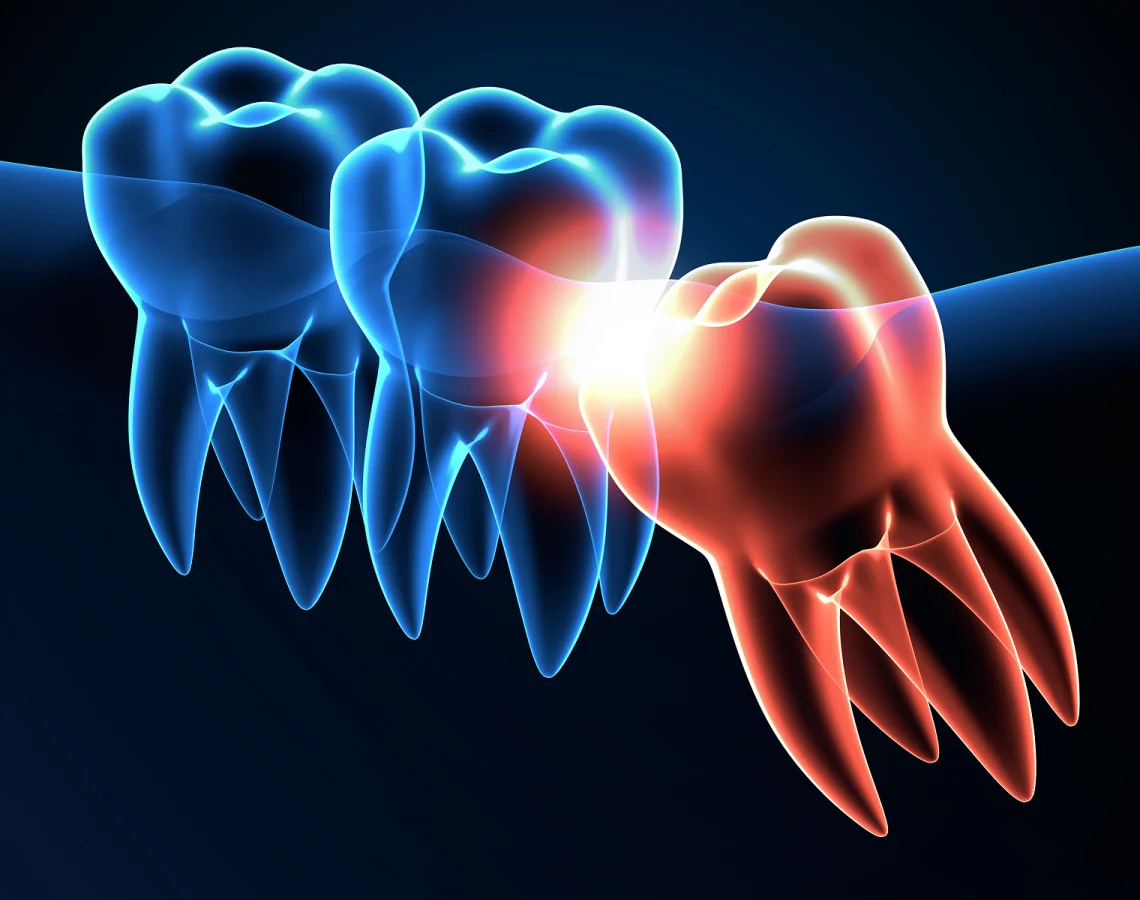
Not every dental issue is an emergency – but if something feels sudden, painful, or worrying, it’s always worth getting checked. Common problems we treat on an emergency basis include:
- Severe toothache or throbbing pain
- Swelling in the face or gums
- Broken or chipped tooth (with or without pain)
- Knocked-out tooth
- Lost crown or filling
- Bleeding or trauma after an accident
- Infections or abscesses
- Jaw pain or difficulty opening the mouth
If you’re unsure whether your situation counts as a dental emergency, call our team – we’ll ask a few quick questions and let you know whether we need to see you the same day or whether a routine appointment is more appropriate.

Emergency Dentist Services We Offer
We provide urgent dental care to both registered and new patients. When you arrive, our goal is to assess the problem, relieve any pain, and offer immediate treatment where possible. Emergency services include:
Pain relief and temporary fillings
Treatment of dental abscesses or infections
Recementing crowns or bridges
Tooth extractions if necessary
Managing cracked or broken teeth
Advice and planning for follow-up treatment
We always aim to resolve the problem in one visit if we can. If further care is needed, we’ll explain everything clearly and schedule follow-up treatment with no pressure.
Emergency Appointments – What to Expect
When you call with a dental emergency, we’ll do our best to offer a same-day appointment – especially for pain, swelling or trauma. If the emergency happens outside our usual hours, our voicemail and website will provide instructions for accessing help.
At your appointment, we’ll carry out a gentle but thorough examination, take X-rays if needed, and give you a clear diagnosis. We’ll treat the immediate problem and advise you on the next steps to ensure long-term relief and recovery.

Why Choose Hampshire Dental Care in a Dental Emergency?
- Same-day emergency appointments available
- Calm, experienced clinicians who listen and act quickly
- Transparent costs and no rushed decisions
- Convenient location near Basingstoke and easy access from Farnham
- Welcoming new and returning patients with or without prior registration
- Full range of follow-up care and treatment options
We know that urgent dental problems are distressing, but you’re in safe hands. We’ll work to relieve your discomfort and give you clear, reassuring answers when you need them most.
Frequently Asked Questions
What should I do if I knock out a tooth?
Keep the tooth (if possible), avoid touching the root, and store it in milk or your saliva. Call us immediately – there’s a better chance of saving it if we see you within an hour.
Can I go to A&E with a dental emergency?
Only if you’re experiencing severe swelling affecting your breathing, heavy bleeding, or facial trauma. For most urgent dental issues, such as pain or broken teeth, an emergency dentist is the best route.
Can you see me if I’m not already a patient?
Yes. We welcome new and unregistered patients for emergency appointments. We’ll ask for a few details when you call and do our best to see you as soon as possible.
Will emergency treatment fix the issue permanently?
Often we can resolve the problem on the day, but sometimes we need to provide temporary relief and schedule follow-up care. We’ll always explain your options clearly.
If you’re in pain or facing a dental problem that can’t wait, call our Basingstoke practice now to speak with our team. We’re here to help you feel better – fast.